A 38-year old patient with a history of myocarditis episode in 2010 (preserved function of left ventricle) was admitted after cardiopulmonary resuscitation (CPR) for ventricular fibrillation (witnessed, 7 minutes basic life support, 10 minutes advanced life support, CPC 1).
Figure 1 ECG on admission with suspicious ST elevations in V1-V2

A transthoracic echocardiography showed only mild LV dysfunction as a consequence of CPR.
Video 1 TTE on admission
.gif)
Coronary angiography on 2nd post-admission day was without pathology.
Video 2 Angiography of the right coronary artery
.gif)
Video 3 Angiography of the left coronary artery
.gif)
Due to pathological ECG pattern in precordial leads and history of ventricular fibrillation, patient was indicated for Ajmaline test.
Figure 2 Ajmaline test (3 minutes) (day 3 after admission)

Figure 3 Ajmaline test (10 minutes) – positive Brugada 1.type in leads V1-V3

Cardiac magnetic resonance showed only discrete area of perimyocarditis in inferolateral part of LV (probably of older date), normal systolic function of both ventricles.
Video 4 CMR 4 chamber view with normal systolic function of both ventricles
.gif)
As a result of a Brugada syndrome diagnosis, a patient was indicated for subcutaneous ICD implantation.
Figure 5 Subcutaneous ICD implantation (day 7 after admission)

Clinical context
The Brugada syndrome is an autosomal dominant genetic disorder with variable expression characterized by abnormal findings on the surface electrocardiogram in conjunction with an increased risk of ventricular tachyarrhythmias and sudden cardiac death.
ECG findings — some form of a pseudo-right bundle branch block and persistent ST segment elevation in leads V1 to V2.
Brugada pattern: patients with typical ECG features who are asymptomatic and have no other clinical criteria.
Brugada syndrome: patients with typical ECG features who have experienced sudden cardiac death or a sustained ventricular tachyarrhythmia, or who have one or more of the other associated clinical criteria (syncope, seizures, and nocturnal agonal respiration due to polymorphic ventricular tachycardia or VF).
1) Type 1 (“coved type”) (Figure 1A): This alteration is the only diagnostic pattern for BrS. It is characterized by an ST-segment elevation ≥2 mm in ≥1 right precordial lead (V1 to V3), followed by an rʹ-wave and a concave or straight ST segment. The descending ST segment crosses the isoelectric line and is followed by a negative and symmetric T-wave.Type 2 Brugada ECG pattern - the ST segment has a "saddle back" ST-T wave configuration
2) Type 2 (“saddle-back type”) (Figure 1B): This ECG anomaly is only suggestive of BrS. It is characterized by an ST-segment elevation ≥0.5 mm (generally ≥2 mm in V2) in ≥1 right precordial lead (V1 to V3), followed by a convex ST. The rʹ-wave may or may not overlap the J point, but it has a slow downward slope. The ST segment is followed by a positive T-wave in V2 and is of variable morphology in V1.
Figure 6

Brugada J, Campuzano O, Arbelo E, et al. Present Status of Brugada Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol 2018; 72:1046.
Learning points
1) Always thoroughly investigate a 12-lead ECG in patients with suspicious episodes of unconsciousness or malignant ventricular tachycardia.
- look for typical ST segment elevations in precordial leads in patients with possible Brugada syndrome.
Where to put chest leads in Brugada syndrome? The placement of the right precordial leads in more cranial positions (in the 3rd or 2nd intercostal spaces) increases sensitivity in some patients due to the variable anatomical correlation between the right ventricular outflow tract and V1 to V2 in the standard position.
2) If you have suspicion on Brugada syndrome, perform a drug challenge:
- Flecainide – 2 mg/kg over 10 minutes intravenously or 400 mg orally
- Procainamide – 10 mg/kg over 10 minutes intravenously
- Ajmaline – 1 mg/kg over 5 minutes intravenously
3) What are the provoking factors of VT/VFib in Brugada patients?
- fever
- medications (tricyclic or tetracyclic antidepressants, lithium)
- metabolic disturbances (severe hyperkalemia)
- toxins - local anesthetics, alcohol or cocaine toxicity
4) What is the treatment?
- Full list medications that have to be avoided: www.brugadadrugs.org
- ICD implantation
- Medical treatment (quinidine, amiodarone)
- Catheter ablation
References
- Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm 2013; 10:1932.
- Brugada J, Campuzano O, Arbelo E, et al. Present Status of Brugada Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol 2018; 72:1046.
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 1992; 20:1391.
- Bayés de Luna A, Brugada J, Baranchuk A, Borggrefe M, Breithardt G, Goldwasser D, Lambiase P, Riera AP, Garcia-Niebla J, Pastore C, Oreto G, McKenna W, Zareba W, Brugada R, Brugada P. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012 Sep;45(5):433-42. doi: 10.1016/j.jelectrocard.2012.06.004. Erratum in: J Electrocardiol. 2013 Jan-Feb;46(1):76. PMID: 22920782.
- Nagase S, Hiramatsu S, Morita H, Nishii N, Murakami M, Nakamura K, Kusano KF, Ito H, Ohe T. Electroanatomical correlation of repolarization abnormalities in Brugada syndrome: detection of type 1 electrocardiogram in the right ventricular outflow tract. J Am Coll Cardiol. 2010 Dec 14;56(25):2143-5. doi: 10.1016/j.jacc.2010.06.050. PMID: 21144977.
- Brugada J, Pappone C, Berruezo A, Vicedomini G, Manguso F, Ciconte G, Giannelli L, Santinelli V. Brugada Syndrome Phenotype Elimination by Epicardial Substrate Ablation. Circ Arrhythm Electrophysiol. 2015 Dec;8(6):1373-81. doi: 10.1161/CIRCEP.115.003220. Epub 2015 Aug 19. PMID: 26291334.
- Rudic B, Chaykovskaya M, Tsyganov A, Kalinin V, Tülümen E, Papavassiliu T, Dösch C, Liebe V, Kuschyk J, Röger S, El-Battrawy I, Akin I, Yakovleva M, Zaklyazminskaya E, Shestak A, Kim S, Chmelevsky M, Borggrefe M. Simultaneous Non-Invasive Epicardial and Endocardial Mapping in Patients With Brugada Syndrome: New Insights Into Arrhythmia Mechanisms. J Am Heart Assoc. 2016 Nov 14;5(11):e004095. doi: 10.1161/JAHA.116.004095. PMID: 27930354; PMCID: PMC5210320.
- UpToDate Brugada syndrome (Epidemiology and pathogenesis, Clinical presentation, diagnosis, and evaluation, Prognosis, management, and approach to screening)
Authors: Michal Pazderník, Tereza Schimerová, Marek Šramko
You Might Also Like
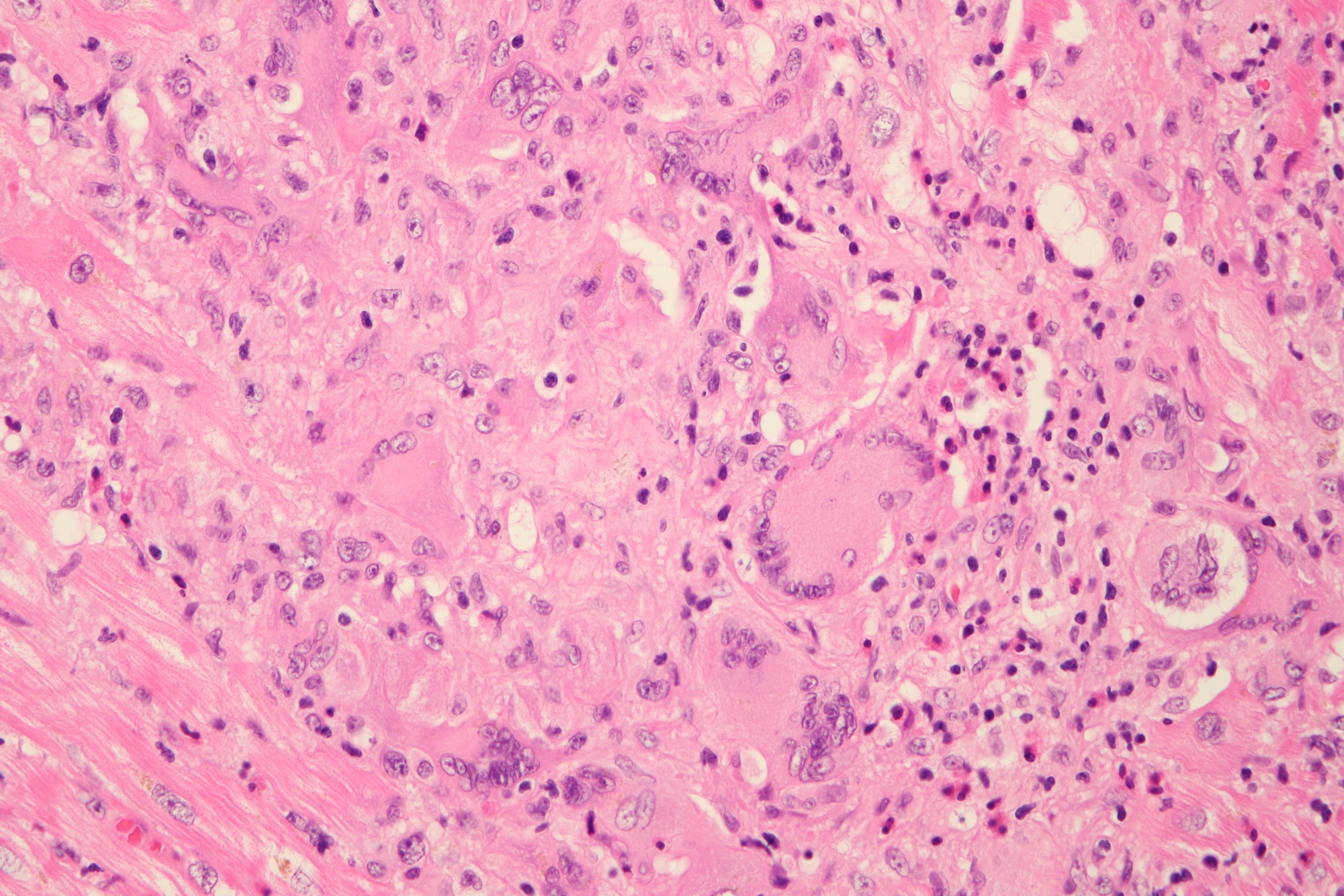
Cardiogenic shock due to Giant Cell Myocarditis
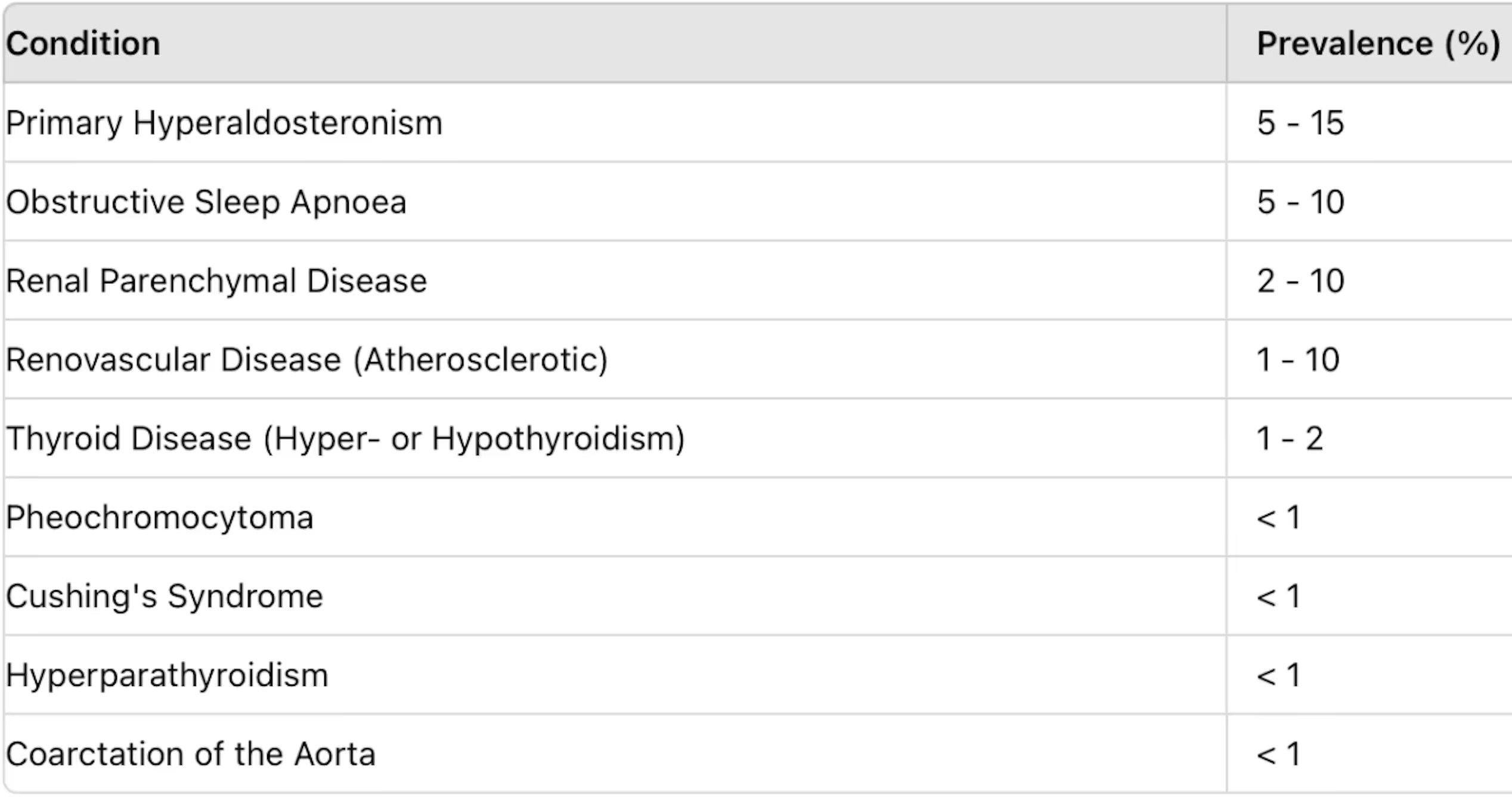
Secondary hypertension


.jpg)


