67-year old man with a history of arterial hypertension, admitted for manifestations of bilateral heart failure caused by atrial fibrillation with a rapid response to ventricles of unknown date of origin (CHADS-VASc 3). Brain natriuretic peptides od admission were 1075 ng/L (normal range, 10-155 ng/L).
Diuretic therapy, anticoagulation and rate control therapy were initiated.
Figure 1 ECG on admission - atrial fibrillation 156/min (RBBB+LAH).

TTE showed severe systolic dysfunction of LV (diffuse hypokinesis, EF=25-30%), dilatation of the right ventricle with moderate dysfunction and bilateral fluidothorax were present.
For an unknown date of atrial fibrillation origin and only partial effect of rate control therapy, the patient was indicated for TEE examination. TEE revealed large highly mobile thrombus (24x14 mm) present in LAA.
Video 1 Transesophageal echocardiography showing massive thrombus in LAA.
.gif)
Video 2 Transesophageal echocardiography showing massive thrombus in LAA.
.gif)
Figure 1 Decreased left atrial appendage emptying velocity documented on TEE (33 cm/s).

Anticoagulation therapy (heparin) was initiated and electrical cardioversion was postponed. Rate control was achieved by maximal tolerated doses of beta blockers and digoxin. Due to presence of extensive pleural effusion, right sided thoracocentesis was done and 1000 ml of transudate was evacuated.
After compensation for acute heart failure, the patient's anticoagulation therapy was converted to NOAC and dismissed to outpatient clinical care with acceptable rate of atrial fibrillation.
Patient was readmitted after 1 month of anticoagulation therapy, repeated TEE was performed.
Transesophageal echocardiography (TEE) documented multilobed akinetic LAA without thrombus.
Video 3 TEE with absence of thrombus in LAA.
.gif)
DC cardioversion of atrial fibrillation was performed successfully to sinus rhythm.
Figure 2 ECG after cardioversion with sinus rhythm (RBBB+LAH).

Clinical context
The left atrial appendage thrombus is a well-known complication of atrial fibrillation and rheumatic mitral valve disease and carries a high risk for systemic thromboembolism.
The LAA is the most prominent site of LA thrombus formation, with more than 90% of thrombi generating within this anatomical structure.
Once a LAA thrombus is identified, therapeutic anticoagulation is recommended for at least three weeks or until LAA thrombus resolution is detected on follow-up TEE.
Learning points
1) Awareness of possible LAA thrombus formation in patients with >48 hours lasting episodes of atrial fibrillation without anticoagulation therapy is of paramount importance before performance of DV version.
2) LAA thrombosis is a contraindication to electrical or pharmacological cardioversion (CV) or catheter ablation (CA) in patients with atrial fibrillation (AF) lasting > 48h without anticoagulation therapy.
3) At least a 3-week course of effective oral anticoagulant therapy is recommended to prevent periprocedural thromboembolism in AF patients scheduled for elective cardioversion.
4) The CHA2DS2-VASc score incorporates the more common stroke risk factors seen in everyday clinical practice, and is recommended to guide anticoagulant therapy in AF patients.
5) Transthoracic echocardiography (TTE) should be performed for the clinical evaluation of every AF patient. TTE provides a comprehensive evaluation of cardiac anatomy and function that can help to define the type of AF and to identify patients with high risk of LAA thrombosis.
6) TEE should be performed in all patients with hemodynamically unstable episodes of atrial fibrillation without a history of effective anticoagulation therapy.
References
- Farkowski MM, Jubele K, Marín F, Gandjbakhch E, Ptaszynski P, Merino JL, Lenarczyk R, Potpara TS. Diagnosis and management of left atrial appendage thrombus in patients with atrial fibrillation undergoing cardioversion or percutaneous left atrial procedures: results of the European Heart Rhythm Association survey. Europace. 2020 Jan 1;22(1):162-169. doi: 10.1093/europace/euz257. PMID: 31501852.
- Melillo E, Palmiero G, Ferro A, Mocavero PE, Monda V, Ascione L. Diagnosis and Management of Left Atrium Appendage Thrombosis in Atrial Fibrillation Patients Undergoing Cardioversion. Medicina (Kaunas). 2019;55(9):511. Published 2019 Aug 21. doi:10.3390/medicina55090511
- Fukunaga M, Masuda H, Isotani A, Morinaga T, Yano M, Miura S, Ando K. Different clinical features between left atrial and left atrial appendage thrombus: an insight into more than 16,000 transesophageal echography database. European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.2388, https://doi.org/10.1093/ehjci/ehaa946.2388
- Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021 Feb 1;42(5):373-498. doi: 10.1093/eurheartj/ehaa612. PMID: 32860505.
Authors: Michal Pazderník, Mariya Kalantay
You Might Also Like
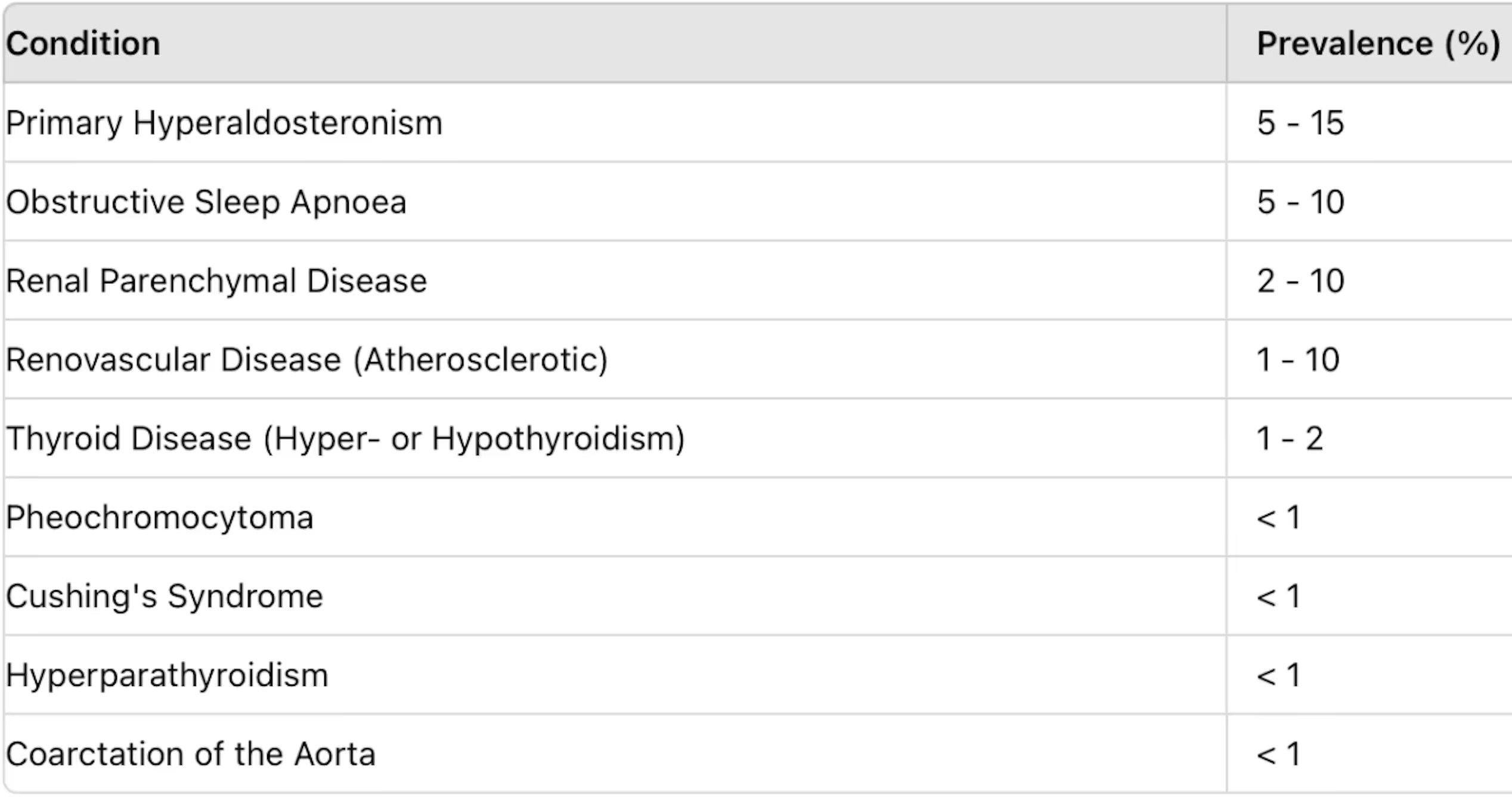
Secondary hypertension

Libman-Sacks endocarditis
.gif)