2.
Fyziologické EKG
3.
EKG obraz základních patologií
4.
Poruchy srdečního rytmu - bradyarytmie
5.
Poruchy srdečního rytmu - tachyarytmie
6.
EKG u infarktu myokardu
7.
Kardiomyopatie, myokarditidy
8.
Pravostranné přetížení srdce
9.
Vrozené arytmické syndromy
10.
Ostatní (Iontové dysbalance, hypotermie a další)
11.
Kardiostimulace
Introduction
Atrial tachycardia (AT) is usually a regular, focal arrhythmia originating in the atrium outside of the sinus node
- mechanism of AT is either a micro-re-entrant circuit or an automatic focus
- ventricular rate is often 130 – 240 beats/min
- AV conduction may be 1:1 or typically 2:1 block or intermittent block
Classification
- Unifocal atrial tachycardia
- Multifocal atrial tachycardia
- irregular atrial rhythm caused by multiple foci within the atrium
- often associated with chronic obstructive lung disease (COPD) or congestive heart failure
ECG:
- atrial rate > 100 beats/min
- at least three P wave morphologies in the same lead
- irregular PP intervals
- the baseline should be isoelectric between P waves
Symptoms
- palpitations
- shortness of breath
- chest pain
- rarely syncope or presyncope
ECG findings
- Regular atrial rate typically 130 – 240 beats/min
- P wave before QRS complex = RP interval is longer than the PR interval
- P waves must be seen and should have isoelectric baseline between them
- P waves have different morphology and axis than sinus rhythm P waves at higher rates – P waves may be embedded in T wave or are completely obscured
- QRS is usually narrow
Finding the site of origin:
P wave morphology
- positive P wave in lead V1 – probable left atrial focus
- positive or biphasic P wave in lead aVL – probable right atrial focus
Causes
- catecholamine surge – enhanced automaticity of a single focus in the atrium takes over pacing from the SA node with warm-up period acceleration to its maximal rate
- in patients with structurally altered atrial tissue (often surgical scars of myocardium) – micro-re-entrant loop around scars with sudden onset and termination
- digoxin in patients with known cardiomyopathy – triggered activity, prolonged tachycardia which is difficult to treat
ECG 1

Atrial tachycardia with 2:1 conduction
- regular narrow complex tachycardia at 115 bpm
- 2:1 = each QRS complex has two P waves – one preceding and one after the QRS

ECG 2

Atrial tachycardia with 2:1 conduction
- regular narrow complex tachycardia at 99 bpm
ECG 3

Atrial tachycardia – anterolateral TRI annulus
- narrow complex tachycardia at 100 bpm
- each QRS complex is preceded by an abnormal P wave – biphasic in lead II, V3, V5, negative in lead V1, aVR

Red arrows – negative P waves in lead V1
ECG 4

Deblocked atrial tachycardia
- regular narrow complex tachycardia at 220 bpm
- deblocked = conduction 1:1
- every QRS complex is preceded with abnormal P wave – best seen in lead V4
- PR interval is shorter than RP interval
Management
Initial treatment of SVT depends on hemodynamic stability of the patient.
- Hemodynamically unstable patient with narrow complex tachycardia – immediate synchronized cardioversion
- Hemodynamically stable patient – Vagal maneuvers and intravenous application of adenosine with continuous ECG monitoring can help with clinical diagnosis. Transient AV block or slowed conduction exposes atrial activity.
Adenosine – through cardiac adenosine A1 receptor > transient AV block demasks atrial activity and in some cases even causes tachycardia termination
- 6 mg i.v. as a rapid bolus with saline flush
- second dose – 12 mg i.v., safe within 1 min of the last dose
- maximum dose = 18 mg
- Adenosine may induce a wide range of transient bradycardias as well as atrial fibrillation, SVT and ventricular tachycardia. Albeit very rare, cases of sustained ventricular tachycardia, ventricular fibrillation and Torsades de pointes have been reported.
Calcium channel blockers (verapamil/diltiazem i.v.)
- Verapamil [0.075 - 0.15 mg/kg i.v. (average 5 - 10 mg) over 2 min] or i.v. diltiazem [0.25 mg/kg (average 20 mg) over 2 min] has been shown to terminate SVT in 64-98% of patients, but is associated with a risk of hypotension.
- application intravenously over 20 minutes has been shown to reduce the rate of hypotension.
Beta blockers
- i.v. esmolol - 0.5 mg/kg i.v. bolus or 0.05 - 0.3 mg/kg/min infusion
- i. v. metoprolol - 2.5-10 mg given i.v. in 2.5 mg boluses
Anticoagulation
- patients with atrial fibrillation, atrial flutter or any supraventricular tachycardia with fast atrial action are at risk of thrombus formation and thromboembolism
- effective anticoagulation is recommended in acute settings pre-cardioversion as well as chronic oral anticoagulation in persistent arrhythmias
- to estimate embolic risk use CHA2DS2-VASc scoring system
- to estimate bleeding risk use HAS-BLED risk score
- oral anticoagulants – warfarin, NOAC (dabigatran, apixaban,..)
- parenteral anticoagulants – unfractionated heparin or low molecular weight heparin
If all pharmacological therapies fail:
Synchronized cardioversion is recommended, even in hemodynamically stable patients
Picture 1 Treatment of focal atrial tachycardia as per ESC guidelines

References
- CAMM, A. J., LÜSCHER, T. F., & SERRUYS, P. W. (2009). The ESC textbook of cardiovascular medicine. Oxford, Oxford University Press
- HARRIGAN, Richard A., William J. BRADY a Theodore C. CHAN. The ECG in Emergency Medicine. Emergency Medicine Clinics of North America [online]. 2006, 24(1) [cit. 2021-01-29]. ISSN 07338627. Dostupné z: doi:10.1016/j.emc.2005.08.001
- Strauss, David G., et al. Marriott's Practical Electrocardiography. Wolters Kluwer, 2021
- Bibas, Lior et al. “Diagnosis and management of supraventricular tachycardias.” CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne vol. 188,17-18 (2016): E466-E473. doi:10.1503/cmaj.160079
- Custer AM, Yelamanchili VS, Lappin SL. Multifocal Atrial Tachycardia. [Updated 2020 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459152/
- Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, Calkins H, Corrado D, Deftereos SG, Diller GP, Gomez-Doblas JJ, Gorenek B, Grace A, Ho SY, Kaski JC, Kuck KH, Lambiase PD, Sacher F, Sarquella-Brugada G, Suwalski P, Zaza A; ESC Scientific Document Group. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020 Feb 1;41(5):655-720. doi: 10.1093/eurheartj/ehz467. PMID: 31504425.
- Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, Campbell WB, Haines DE, Kuck KH, Lerman BB, Miller DD, Shaeffer CW, Stevenson WG, Tomaselli GF, Antman EM, Smith SC Jr, Alpert JS, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Hiratzka LF, Hunt SA, Jacobs AK, Russell RO Jr, Priori SG, Blanc JJ, Budaj A, Burgos EF, Cowie M, Deckers JW, Garcia MA, Klein WW, Lekakis J, Lindahl B, Mazzotta G, Morais JC, Oto A, Smiseth O, Trappe HJ; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias--executive summary. a report of the American college of cardiology/American heart association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003 Oct 15;42(8):1493-531. doi: 10.1016/j.jacc.2003.08.013. PMID: 14563598.

Introduction
Atrial tachycardia (AT) is usually a regular, focal arrhythmia originating in the atrium outside of the sinus node
- mechanism of AT is either a micro-re-entrant circuit or an automatic focus
- ventricular rate is often 130 – 240 beats/min
- AV conduction may be 1:1 or typically 2:1 block or intermittent block
Classification
- Unifocal atrial tachycardia
- Multifocal atrial tachycardia
- irregular atrial rhythm caused by multiple foci within the atrium
- often associated with chronic obstructive lung disease (COPD) or congestive heart failure
ECG:
- atrial rate > 100 beats/min
- at least three P wave morphologies in the same lead
- irregular PP intervals
- the baseline should be isoelectric between P waves
Symptoms
- palpitations
- shortness of breath
- chest pain
- rarely syncope or presyncope
ECG findings
- Regular atrial rate typically 130 – 240 beats/min
- P wave before QRS complex = RP interval is longer than the PR interval
- P waves must be seen and should have isoelectric baseline between them
- P waves have different morphology and axis than sinus rhythm P waves at higher rates – P waves may be embedded in T wave or are completely obscured
- QRS is usually narrow
Finding the site of origin:
P wave morphology
- positive P wave in lead V1 – probable left atrial focus
- positive or biphasic P wave in lead aVL – probable right atrial focus
Causes
- catecholamine surge – enhanced automaticity of a single focus in the atrium takes over pacing from the SA node with warm-up period acceleration to its maximal rate
- in patients with structurally altered atrial tissue (often surgical scars of myocardium) – micro-re-entrant loop around scars with sudden onset and termination
- digoxin in patients with known cardiomyopathy – triggered activity, prolonged tachycardia which is difficult to treat
ECG 1

Atrial tachycardia with 2:1 conduction
- regular narrow complex tachycardia at 115 bpm
- 2:1 = each QRS complex has two P waves – one preceding and one after the QRS

ECG 2

Atrial tachycardia with 2:1 conduction
- regular narrow complex tachycardia at 99 bpm
ECG 3

Atrial tachycardia – anterolateral TRI annulus
- narrow complex tachycardia at 100 bpm
- each QRS complex is preceded by an abnormal P wave – biphasic in lead II, V3, V5, negative in lead V1, aVR

Red arrows – negative P waves in lead V1
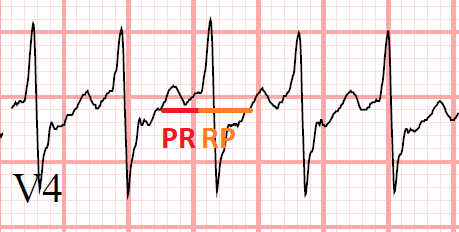
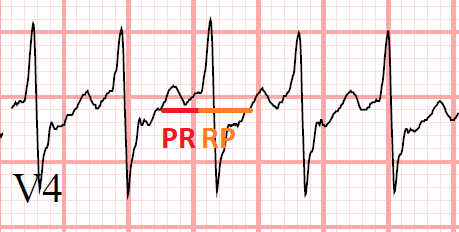
ECG 4

Deblocked atrial tachycardia
- regular narrow complex tachycardia at 220 bpm
- deblocked = conduction 1:1
- every QRS complex is preceded with abnormal P wave – best seen in lead V4
- PR interval is shorter than RP interval
Management
Initial treatment of SVT depends on hemodynamic stability of the patient.
- Hemodynamically unstable patient with narrow complex tachycardia – immediate synchronized cardioversion
- Hemodynamically stable patient – Vagal maneuvers and intravenous application of adenosine with continuous ECG monitoring can help with clinical diagnosis. Transient AV block or slowed conduction exposes atrial activity.
Adenosine – through cardiac adenosine A1 receptor > transient AV block demasks atrial activity and in some cases even causes tachycardia termination
- 6 mg i.v. as a rapid bolus with saline flush
- second dose – 12 mg i.v., safe within 1 min of the last dose
- maximum dose = 18 mg
- Adenosine may induce a wide range of transient bradycardias as well as atrial fibrillation, SVT and ventricular tachycardia. Albeit very rare, cases of sustained ventricular tachycardia, ventricular fibrillation and Torsades de pointes have been reported.
Calcium channel blockers (verapamil/diltiazem i.v.)
- Verapamil [0.075 - 0.15 mg/kg i.v. (average 5 - 10 mg) over 2 min] or i.v. diltiazem [0.25 mg/kg (average 20 mg) over 2 min] has been shown to terminate SVT in 64-98% of patients, but is associated with a risk of hypotension.
- application intravenously over 20 minutes has been shown to reduce the rate of hypotension.
Beta blockers
- i.v. esmolol - 0.5 mg/kg i.v. bolus or 0.05 - 0.3 mg/kg/min infusion
- i. v. metoprolol - 2.5-10 mg given i.v. in 2.5 mg boluses
Anticoagulation
- patients with atrial fibrillation, atrial flutter or any supraventricular tachycardia with fast atrial action are at risk of thrombus formation and thromboembolism
- effective anticoagulation is recommended in acute settings pre-cardioversion as well as chronic oral anticoagulation in persistent arrhythmias
- to estimate embolic risk use CHA2DS2-VASc scoring system
- to estimate bleeding risk use HAS-BLED risk score
- oral anticoagulants – warfarin, NOAC (dabigatran, apixaban,..)
- parenteral anticoagulants – unfractionated heparin or low molecular weight heparin
If all pharmacological therapies fail:
Synchronized cardioversion is recommended, even in hemodynamically stable patients
Picture 1 Treatment of focal atrial tachycardia as per ESC guidelines

References
- CAMM, A. J., LÜSCHER, T. F., & SERRUYS, P. W. (2009). The ESC textbook of cardiovascular medicine. Oxford, Oxford University Press
- HARRIGAN, Richard A., William J. BRADY a Theodore C. CHAN. The ECG in Emergency Medicine. Emergency Medicine Clinics of North America [online]. 2006, 24(1) [cit. 2021-01-29]. ISSN 07338627. Dostupné z: doi:10.1016/j.emc.2005.08.001
- Strauss, David G., et al. Marriott's Practical Electrocardiography. Wolters Kluwer, 2021
- Bibas, Lior et al. “Diagnosis and management of supraventricular tachycardias.” CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne vol. 188,17-18 (2016): E466-E473. doi:10.1503/cmaj.160079
- Custer AM, Yelamanchili VS, Lappin SL. Multifocal Atrial Tachycardia. [Updated 2020 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459152/
- Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, Calkins H, Corrado D, Deftereos SG, Diller GP, Gomez-Doblas JJ, Gorenek B, Grace A, Ho SY, Kaski JC, Kuck KH, Lambiase PD, Sacher F, Sarquella-Brugada G, Suwalski P, Zaza A; ESC Scientific Document Group. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020 Feb 1;41(5):655-720. doi: 10.1093/eurheartj/ehz467. PMID: 31504425.
- Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, Campbell WB, Haines DE, Kuck KH, Lerman BB, Miller DD, Shaeffer CW, Stevenson WG, Tomaselli GF, Antman EM, Smith SC Jr, Alpert JS, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Hiratzka LF, Hunt SA, Jacobs AK, Russell RO Jr, Priori SG, Blanc JJ, Budaj A, Burgos EF, Cowie M, Deckers JW, Garcia MA, Klein WW, Lekakis J, Lindahl B, Mazzotta G, Morais JC, Oto A, Smiseth O, Trappe HJ; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias--executive summary. a report of the American college of cardiology/American heart association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003 Oct 15;42(8):1493-531. doi: 10.1016/j.jacc.2003.08.013. PMID: 14563598.






