2.
Fyziologické EKG
3.
EKG obraz základních patologií
4.
Poruchy srdečního rytmu - bradyarytmie
5.
Poruchy srdečního rytmu - tachyarytmie
6.
EKG u infarktu myokardu
7.
Kardiomyopatie, myokarditidy
8.
Pravostranné přetížení srdce
9.
Vrozené arytmické syndromy
10.
Ostatní (Iontové dysbalance, hypotermie a další)
11.
Kardiostimulace
Alternative names include Idiopathic Fascicular Left Ventricular Tachycardia (IFLVT), Belhassen-type VT, verapamil-sensitive VT.
Introduction
- Fascicular VT was originally described by Zipes et al (1979) and treatment with verapamil was suggested by Belhassen et al (1981)
- It is the second most common cause of idiopathic left ventricular tachycardia, which is defined as VT that occurs in patients without structural heart disease, metabolic abnormalities, or the long QT syndrome.
- It typically occurs in young adult patients without structural heart disease and it predominantly affects men (60-80%)
- Typical clinical presentation includes palpitations, dizziness or syncope. It usually occurs at rest but it can also be triggered by exercise, emotional stress and catecholamine infusion
- It is a reentrant tachycardia with the reentry circuit comprising interventricular septum and fascicular system
ECG characteristics
- monomorphic VT with typical features of VT such as AV dissociation, possible presence of fusion beats and other ECG signs
- VT with a relatively narrow QRS complex that usually doesn’t exceed 140-150 ms and RS of 60-80 ms
- Typically having RBBB morphology
- Immediately after tachycardia termination, T wave inversion may be present.
- Because of its narrow QRS complex morphology it can be mistaken for SVT conducted with aberrancy. It must also be distinguished from other narrow complex VTs.
Classification
- a) Posterior fascicular ventricular tachycardia - is the most common type (90-95% of cases) and it uses the posterior fascicle as part of its circuit. It is characterised by RBBB morphology and left axis deviation.
- b) Anterior fascicular ventricular tachycardia - is less frequent and it uses the anterior fascicle as part of its circuit. It is characterised by RBBB morphology and right axis deviation.
- c) Upper septal fascicular ventricular tachycardia is a rare variant that usually presents as RBBB morphology but cases resembling LBBB have been described.
Management
- In acute situations when the patient is hemodynamically unstable and/or does not tolerate the IFLVT, electrical cardioversion is recommended
- In case when the patient does not require electrical cardioversion, administration of verapamil is effective in terminating the arrhythmia
- IFLVT usually does not respond to vagal manoeuvres, adenosine or beta blockers
- Currently recommended first-line treatment is catheter ablation in experienced centres. This is based on the fact that long-term verapamil treatment is not effective. Success rate of catheter ablation is 85-95% and recurrence is present in 0-20% of patients
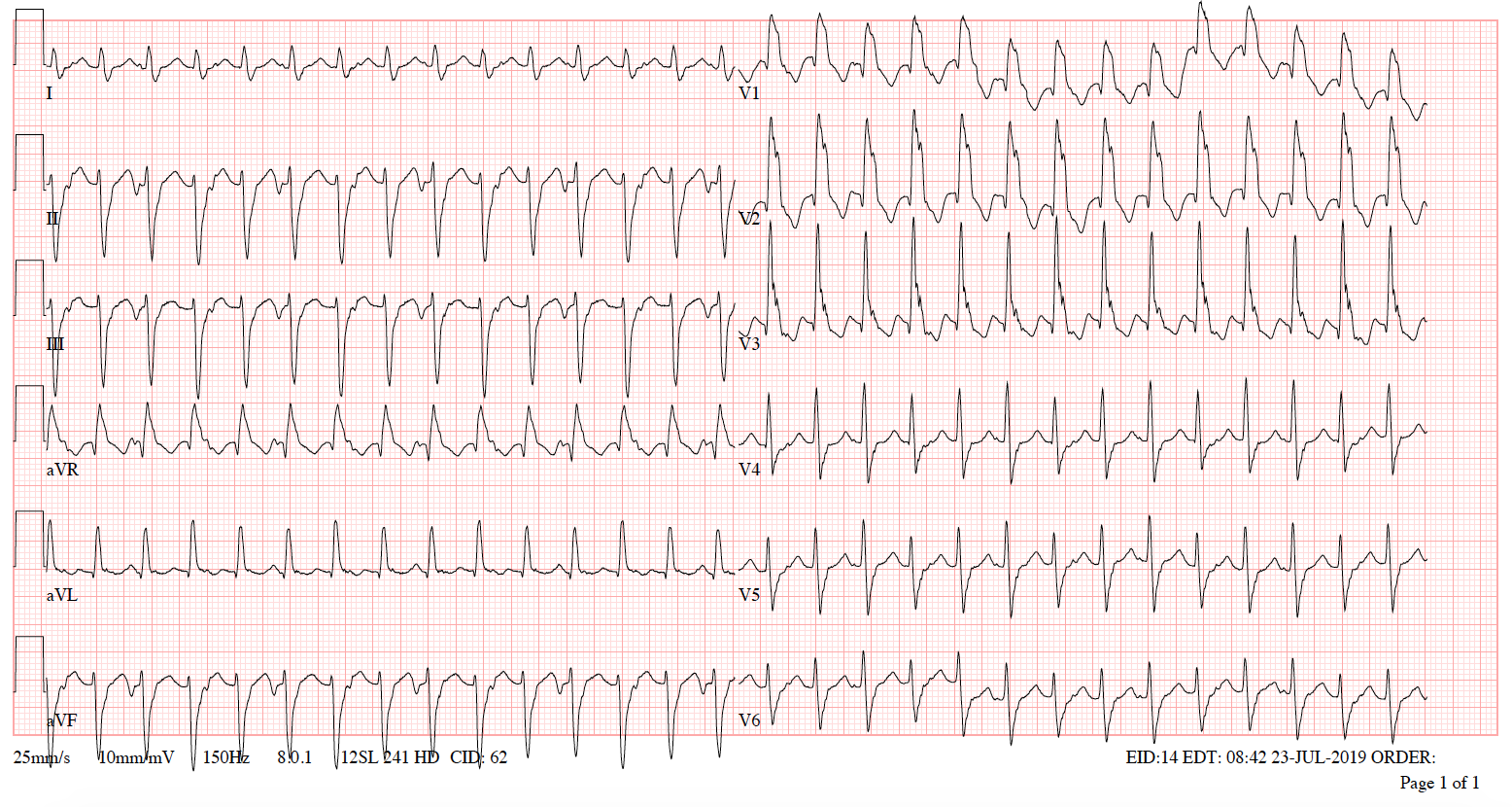
ECG 1A Monomorphic VT (posterior fascicular ventricular tachycardia) with a ventricular rate of 176/min and a narrow QRS (116ms), RBBB morphology + left axis deviation

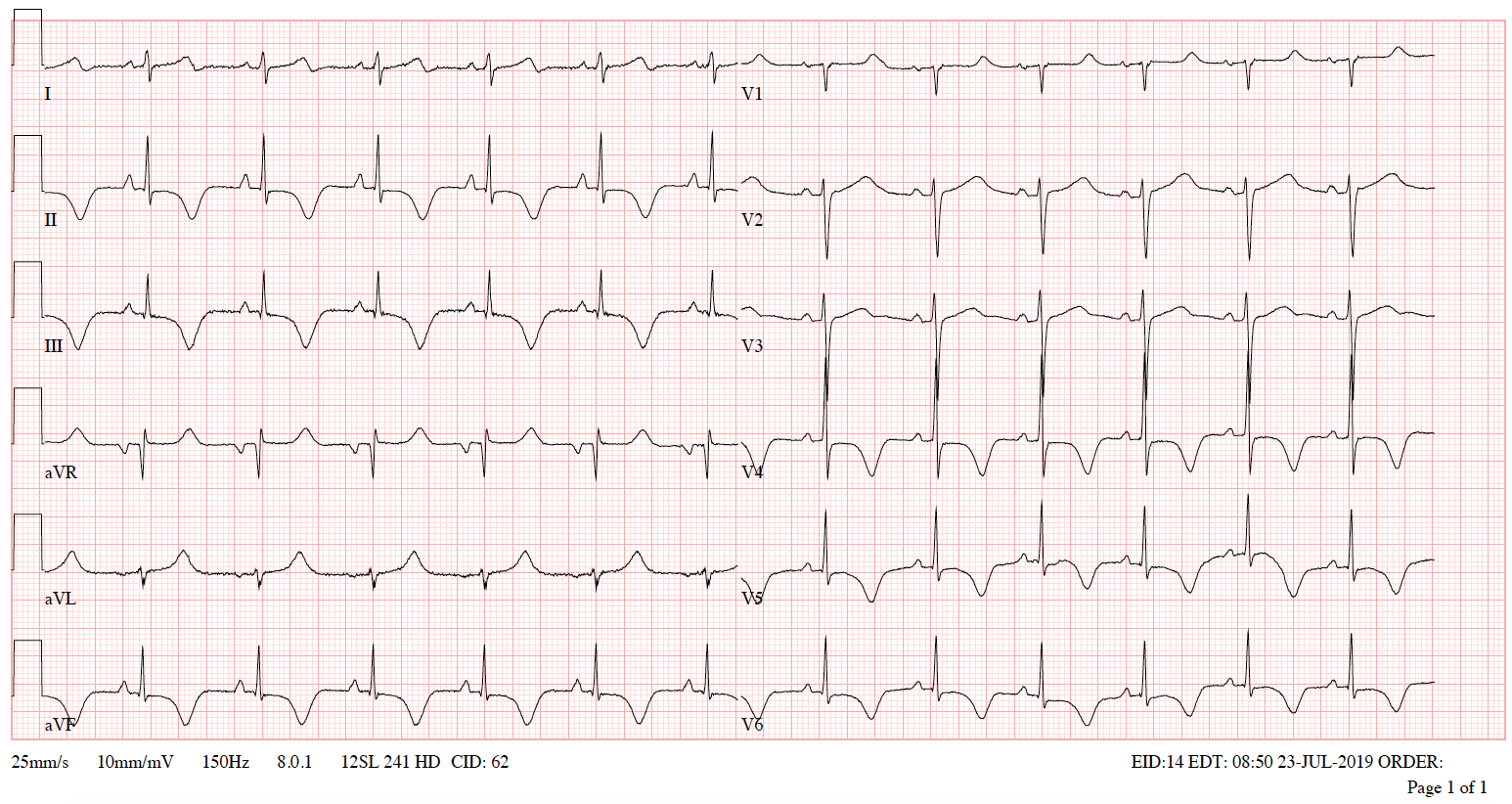
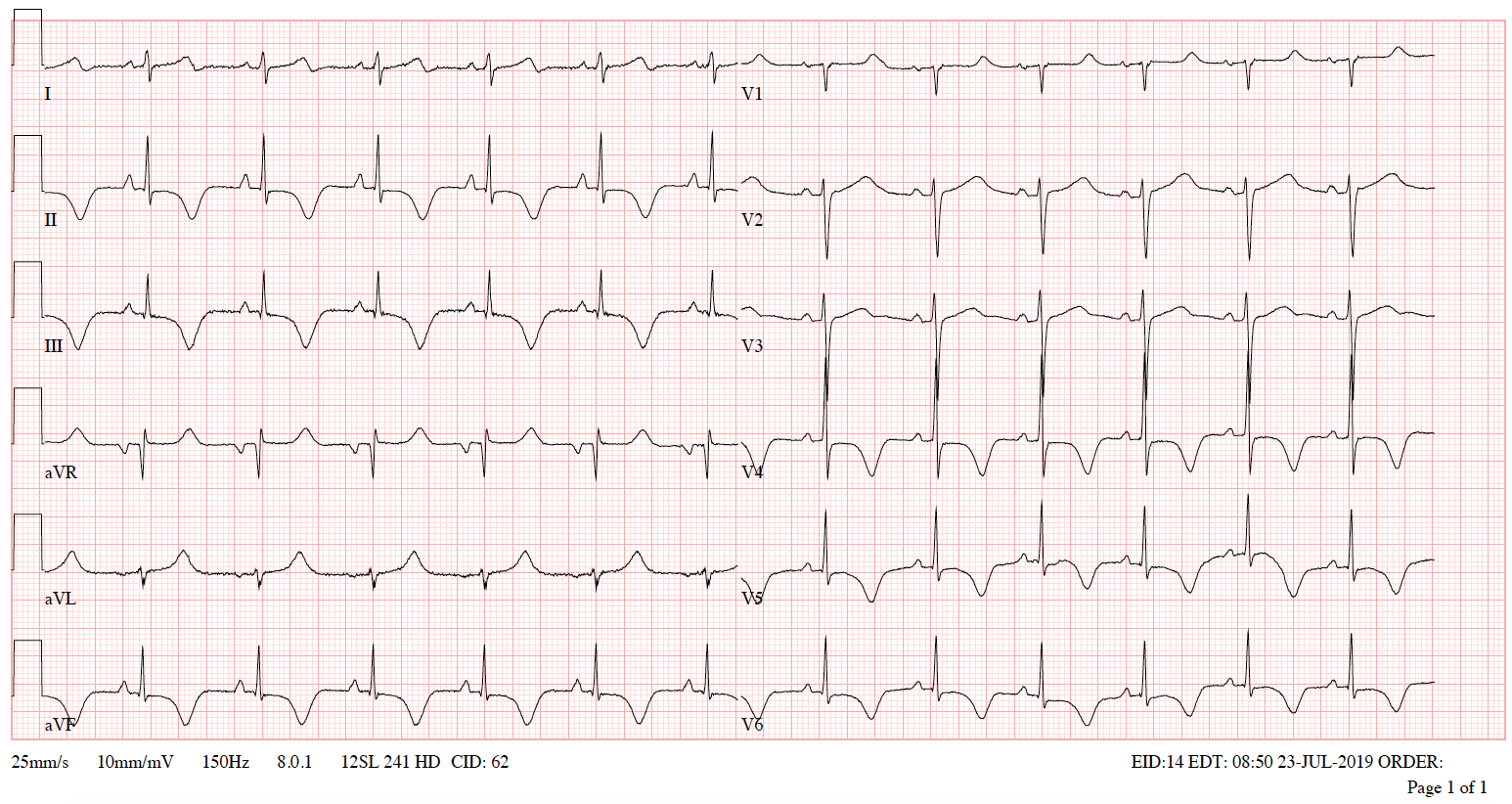
ECG 1B VT after termination
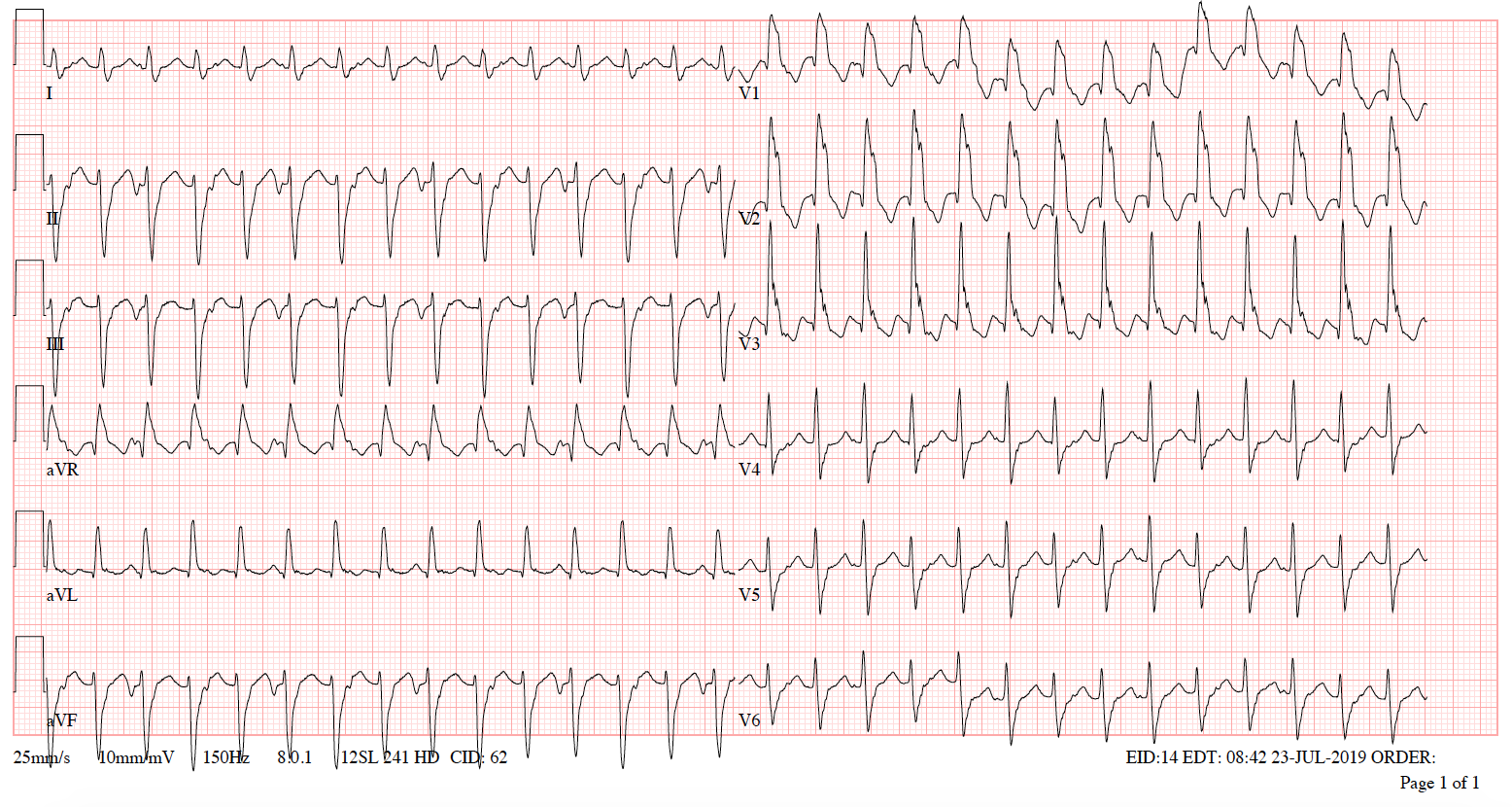
ECG 2 Monomorphic VT (posterior fascicular ventricular tachycardia) with a ventricular rate of 174/min and QRS duration of 128ms, RBBB morphology + left axis deviation
References
- Idiopathic fascicular left ventricular tachycardia, An article from the E-Journal of the ESC
- Council for Cardiology Practice Vol. 9, N° 13 - 20 Dec 2010, Dr. Sara Moreno Reviriego
- LITFL: https://litfl.com/idiopathic-fascicular-left-ventricular-tachycardia/
- How to recognise and manage idiopathic ventricular tachycardia (escardio.org)
- Zipes D. P., Foster P. R., Troup P. J. et al. Atrial induction of ventricular tachycardia: reentry versus triggered automaticity. Am J Cardiol, 1979. 44: 1-8. 10.
- Belhassen B., Rotmensch H. H., & Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J, 1981. 46: 679-82.
- Kapa S, Gaba P, DeSimone CV, Asirvatham SJ. Fascicular Ventricular Arrhythmias: Pathophysiologic Mechanisms, Anatomical Constructs, and Advances in Approaches to Management. Circ Arrhythm Electrophysiol. 2017 Jan;10(1):e002476. doi: 10.1161/CIRCEP.116.002476. PMID: 28087563.
- Silvia G Priori, Carina Blomström-Lundqvist, Andrea Mazzanti et al. ESC Scientific Document Group, 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), European Heart Journal, Volume 36, Issue 41, 1 November 2015, Pages 2793–2867, https://doi.org/10.1093/eurheartj/ehv316

Alternative names include Idiopathic Fascicular Left Ventricular Tachycardia (IFLVT), Belhassen-type VT, verapamil-sensitive VT.
Introduction
- Fascicular VT was originally described by Zipes et al (1979) and treatment with verapamil was suggested by Belhassen et al (1981)
- It is the second most common cause of idiopathic left ventricular tachycardia, which is defined as VT that occurs in patients without structural heart disease, metabolic abnormalities, or the long QT syndrome.
- It typically occurs in young adult patients without structural heart disease and it predominantly affects men (60-80%)
- Typical clinical presentation includes palpitations, dizziness or syncope. It usually occurs at rest but it can also be triggered by exercise, emotional stress and catecholamine infusion
- It is a reentrant tachycardia with the reentry circuit comprising interventricular septum and fascicular system
ECG characteristics
- monomorphic VT with typical features of VT such as AV dissociation, possible presence of fusion beats and other ECG signs
- VT with a relatively narrow QRS complex that usually doesn’t exceed 140-150 ms and RS of 60-80 ms
- Typically having RBBB morphology
- Immediately after tachycardia termination, T wave inversion may be present.
- Because of its narrow QRS complex morphology it can be mistaken for SVT conducted with aberrancy. It must also be distinguished from other narrow complex VTs.
Classification
- a) Posterior fascicular ventricular tachycardia - is the most common type (90-95% of cases) and it uses the posterior fascicle as part of its circuit. It is characterised by RBBB morphology and left axis deviation.
- b) Anterior fascicular ventricular tachycardia - is less frequent and it uses the anterior fascicle as part of its circuit. It is characterised by RBBB morphology and right axis deviation.
- c) Upper septal fascicular ventricular tachycardia is a rare variant that usually presents as RBBB morphology but cases resembling LBBB have been described.
Management
- In acute situations when the patient is hemodynamically unstable and/or does not tolerate the IFLVT, electrical cardioversion is recommended
- In case when the patient does not require electrical cardioversion, administration of verapamil is effective in terminating the arrhythmia
- IFLVT usually does not respond to vagal manoeuvres, adenosine or beta blockers
- Currently recommended first-line treatment is catheter ablation in experienced centres. This is based on the fact that long-term verapamil treatment is not effective. Success rate of catheter ablation is 85-95% and recurrence is present in 0-20% of patients
ECG 1A Monomorphic VT (posterior fascicular ventricular tachycardia) with a ventricular rate of 176/min and a narrow QRS (116ms), RBBB morphology + left axis deviation

ECG 1B VT after termination
ECG 2 Monomorphic VT (posterior fascicular ventricular tachycardia) with a ventricular rate of 174/min and QRS duration of 128ms, RBBB morphology + left axis deviation
References
- Idiopathic fascicular left ventricular tachycardia, An article from the E-Journal of the ESC
- Council for Cardiology Practice Vol. 9, N° 13 - 20 Dec 2010, Dr. Sara Moreno Reviriego
- LITFL: https://litfl.com/idiopathic-fascicular-left-ventricular-tachycardia/
- How to recognise and manage idiopathic ventricular tachycardia (escardio.org)
- Zipes D. P., Foster P. R., Troup P. J. et al. Atrial induction of ventricular tachycardia: reentry versus triggered automaticity. Am J Cardiol, 1979. 44: 1-8. 10.
- Belhassen B., Rotmensch H. H., & Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J, 1981. 46: 679-82.
- Kapa S, Gaba P, DeSimone CV, Asirvatham SJ. Fascicular Ventricular Arrhythmias: Pathophysiologic Mechanisms, Anatomical Constructs, and Advances in Approaches to Management. Circ Arrhythm Electrophysiol. 2017 Jan;10(1):e002476. doi: 10.1161/CIRCEP.116.002476. PMID: 28087563.
- Silvia G Priori, Carina Blomström-Lundqvist, Andrea Mazzanti et al. ESC Scientific Document Group, 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), European Heart Journal, Volume 36, Issue 41, 1 November 2015, Pages 2793–2867, https://doi.org/10.1093/eurheartj/ehv316






