2.
Fyziologické EKG
3.
EKG obraz základních patologií
4.
Poruchy srdečního rytmu - bradyarytmie
5.
Poruchy srdečního rytmu - tachyarytmie
6.
EKG u infarktu myokardu
7.
Kardiomyopatie, myokarditidy
8.
Pravostranné přetížení srdce
9.
Vrozené arytmické syndromy
10.
Ostatní (Iontové dysbalance, hypotermie a další)
11.
Kardiostimulace
Introduction
- Outflow tract ventricular tachycardias (OTVT) are the most common cause of idiopathic ventricular tachycardias followed by fascicular tachycardias
- Structural heart disease must be ruled out as OTVT tachycardias can manifest in patients with underlying heart disease such as myocardial infarction, arrhythmogenic cardiomyopathy or sarcoidosis
- In the absence of structural heart disease the prognosis is good
- Management of OTVT differs in RVOT and LVOT tachycardias
- The region of outflow tracts is anatomically complex and many structures can give rise to arrhythmias and precise determination of the origin may be possible only during electrophysiological study
Classification
- two types of OTVT can be distinguished:
- Paroxysmal OTVT is typically triggered by exercise or stress
- Repetitive monomorphic OTVT usually occurs at rest and presents with runs of nonsustained VTs interrupted by sinus beats
Right Ventricular Outflow Tract VT/PVC
Introduction
- RVOT is the most common origin of idiopathic VT, it represents approximately 70% of VTs in patients with structurally normal hearts and 10% of all VTs
- RVOT VT typically presents in patients 20-50 years old and affects more frequently women
- RVOT VT can also occur in patients with arrhythmogenic cardiomyopathy as the right ventricle is the most common localisation (ARVC arrhythmias do not terminate with adenosine)
- Clinical presentation can vary and it can be asymptomatic or present with palpitations or syncope. RVOT VT presents with syncope more often than LVOT VT
ECG characteristics
- Localising RVOT VT may be difficult due to the proximity of several structures acting as potential origin of outflow tract VTs (RVOT, LVOT, cusps of aortic valve, great cardiac veins, epicardial myocardium, aortomitral continuity and rarely pulmonary artery)
- Apart from typical features of a VT, the following ECG features are used to localise RVOT VT/PVCs:
- LBBB morphology
- Inferior axis
- Anterior sites in the RVOT show a dominant Q-wave or a qR complex in lead I and a QS complex in aVL. Pacing at the posterior sites produces a dominant R-wave in lead I, QS or R-wave in aVL and an early precordial transition (R/S = 1 by V3)
- Precordial transition in V3 or later and shorter R wave duration in V1 and V2 (distinguishes RVOT origin from LVOT)
- If multiple morphologies are present, scar related VT as in arrhythmogenic cardiomyopathy should be suspected
Management
- Outflow tract VT can usually be terminated by either vagal manoeuvres, adenosine or verapamil
- In symptomatic patients with RVOT VT or PVCs, catheter ablation can be highly effective and is a recommended treatment (targeting the earliest high-frequency Purkinje potential during VT)
- Patients with moderate symptoms can be treated with oral verapamil (120 mg/day to 480 mg/day)
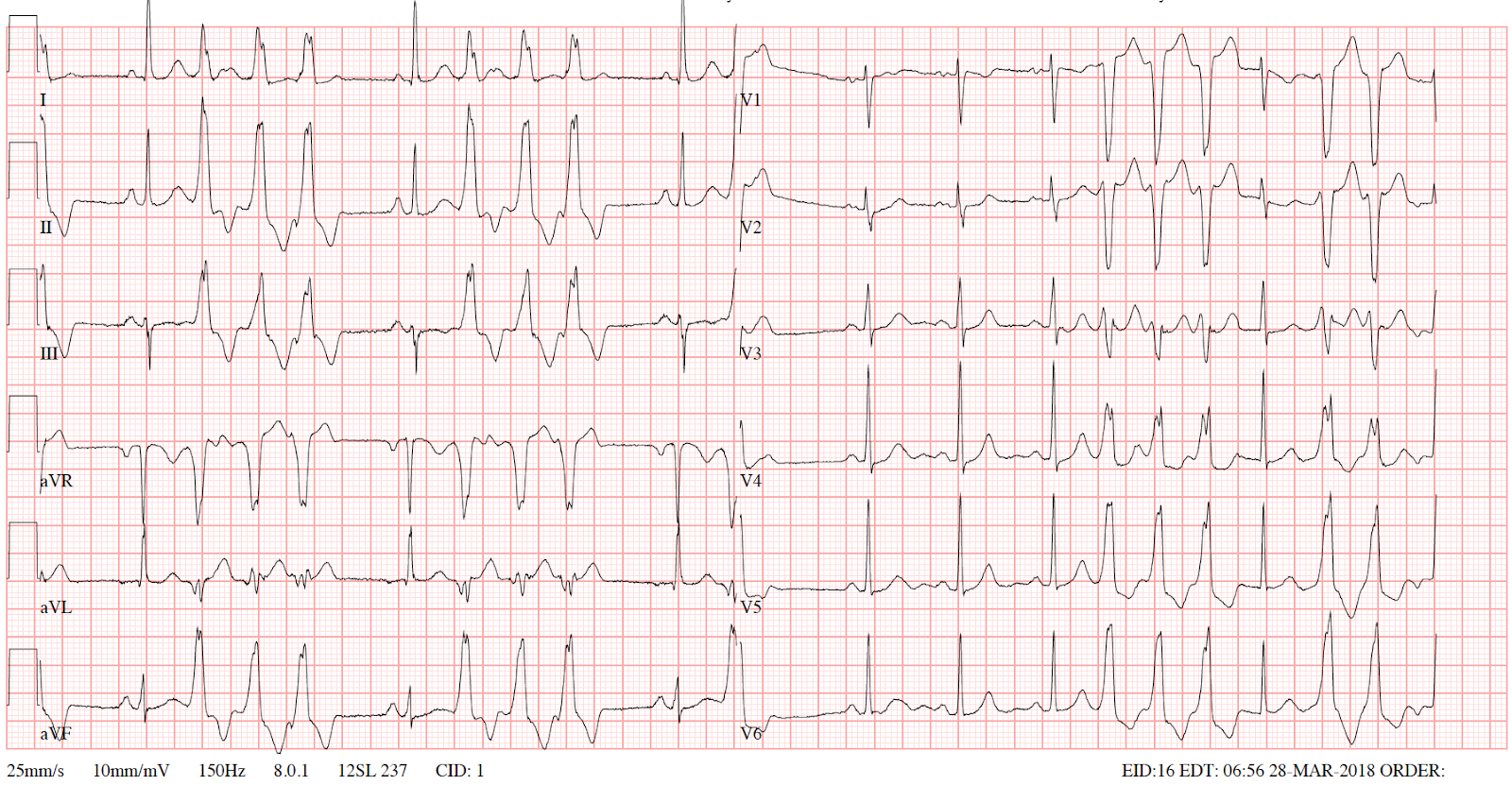
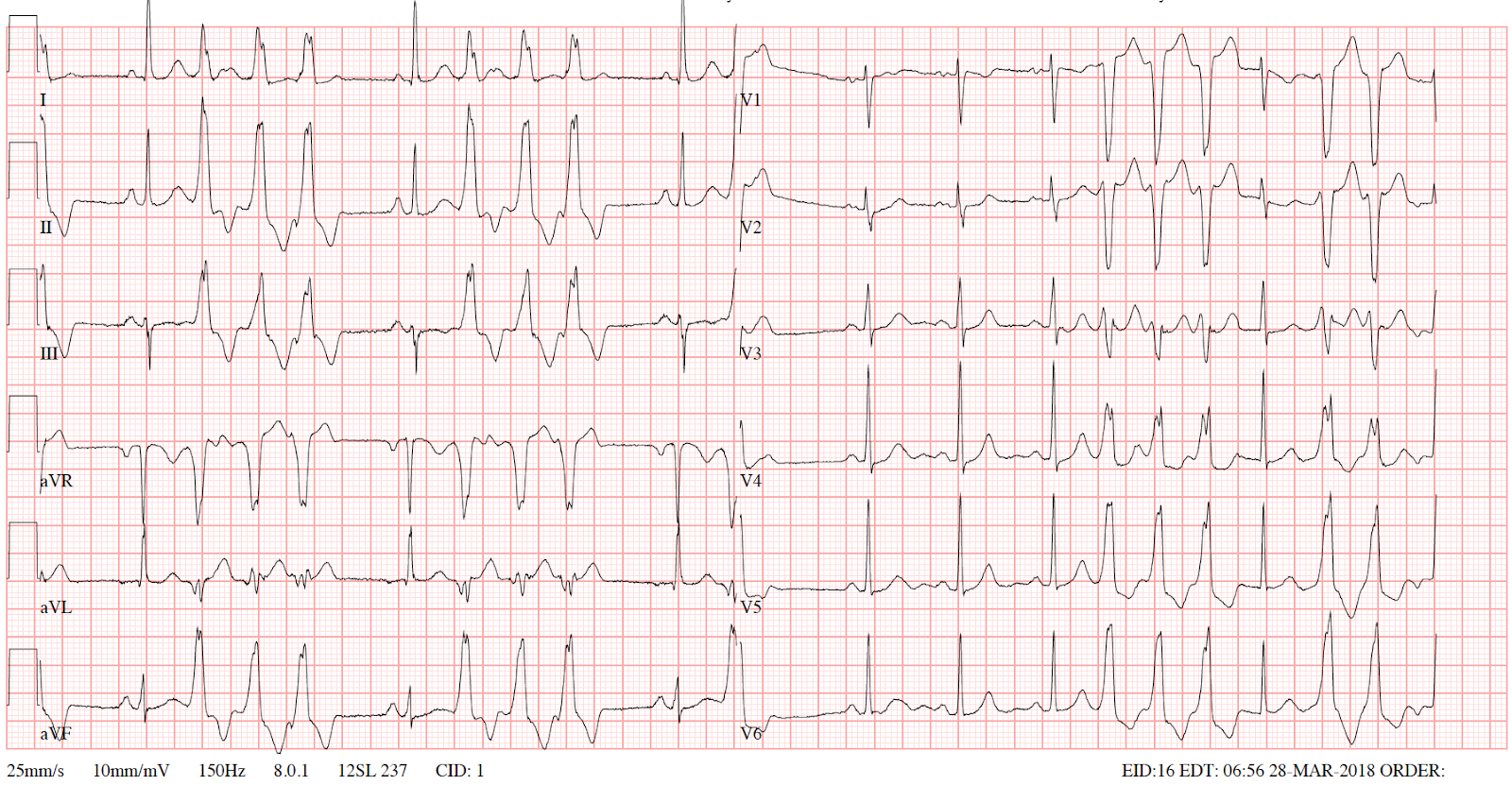
ECG 1
- runs of non sustained VT from RVOT with interposed sinus beats
- LBBB morphology
- inferior axis (positive QRS complex in II, III and aVF)
- precordial transition in V4

ECG 2
- triplets of PVCs from RVOT
- LBBB morphology
- inferior axis
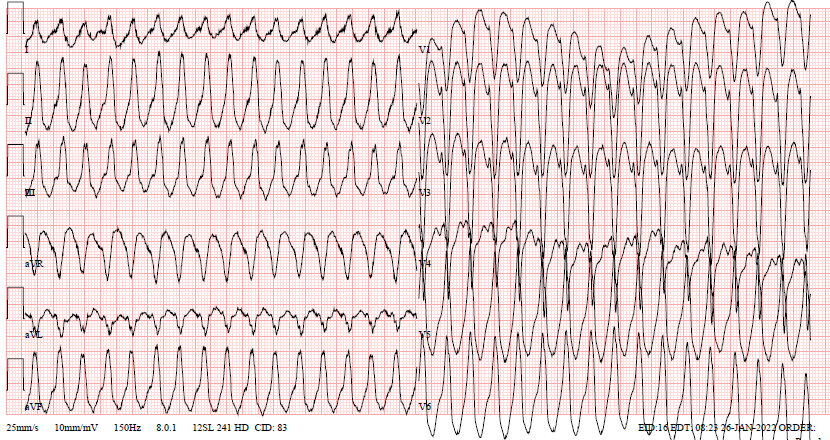
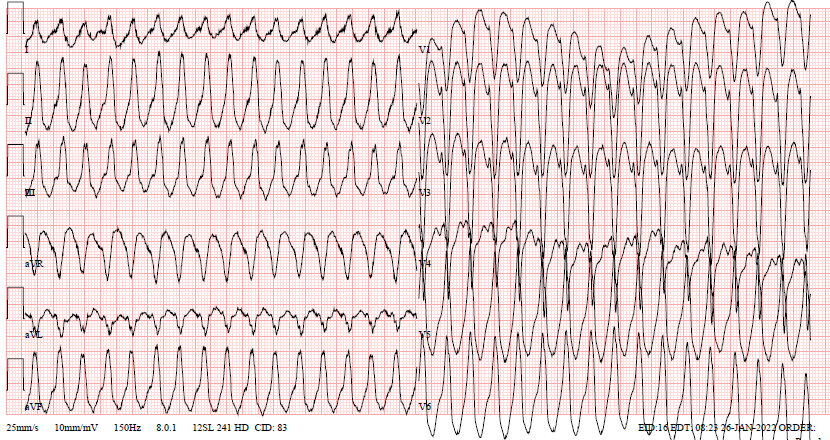
ECG 3 RVOT ventricular tachycardia (LBBB + inferior axis)
Left ventricular outflow tract VT
Introduction
- LVOT VTs account for about 10-15% of idiopathic VTs
- LVOT origin can be divided into more precise localisation including the aorto-mitral continuity (AMC), the anterior site around the mitral annulus (MA), the aortic sinus cusps (ASC), and the epicardium although these localisations are sometimes considered separately
- All of these sites of origin exhibit similar morphology due to their close anatomical proximity
- There are algorithms that can be used to precisely localise the origin of LVOT VT/PVC and it can be used in the decision to perform a catheter ablation as not all of the mentioned localisations can be successfully ablated.
ECG characteristics
- LVOT VT is suggested by LBBB morphology with inferior axis with small R-waves in V1 and early precordial transition (R/S = 1 by V2 or V3) or RBBB morphology with inferior axis and presence of S-wave in V6 (4).
- inferior axis (positive deflections in leads II, III and aVF)
- Aortic sinus cusp origin is sometimes difficult to differentiate from RVOT VT because both are so close to each other. Coronary cusp origin has to be thought when we fail an ablation in the RVOT, ECG shows a LBBB inferior axis morphology with taller monophasic R-waves in inferior leads and an early precordial R-wave transition by V2-V3.
Management
- if stable, utilize vagal maneuvers, adenosine, and/or verapamil
- chronic therapy involves beta blockers, non-dihydropyridines, class IC agents (sodium channel blockers)
- Curative catheter ablation should be considered, however, success rate of catheter ablation is lower than in the case RVOT VT/PVC and can have major complications and should therefore be performed only in highly experienced centres
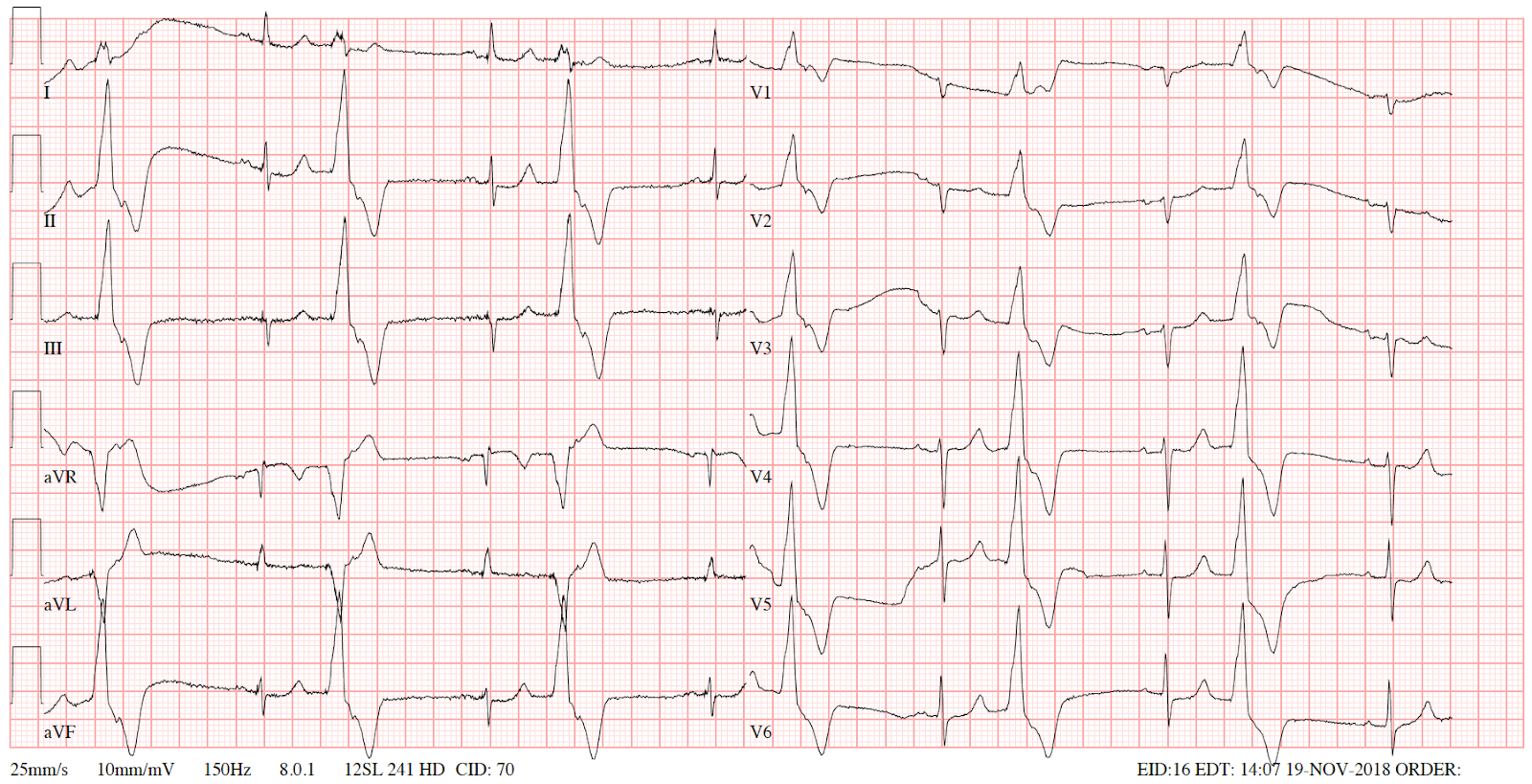
ECG 1 Trigeminy of PVCs from commissure of right and left aortic cusps (curative ablation done)

ECG 2 Bigeminy originating from LVOT (curative ablation done)
- bigeminy with PVCs of RBBB morphology in V1
- inferior axis (positive deflection in leads II, III and aVF)
References
- Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 11th ed, Zipes DP, Libby P, Bonow RO, et al, W.B. Saunders Company, Philadelphia 2018.
- Silvia G Priori, Carina Blomström-Lundqvist, Andrea Mazzanti et al. ESC Scientific Document Group, 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), European Heart Journal, Volume 36, Issue 41, 1 November 2015, Pages 2793–2867, https://doi.org/10.1093/eurheartj/ehv316
- Right Ventricular Outflow Tract (RVOT) Tachycardia • LITFL • ECG Library
- Kumagai, Koji. 2014. “Idiopathic Ventricular Arrhythmias Arising From The Left Ventricular Outflow Tract: Tips And Tricks”. Journal Of Arrhythmia 30 (4): 211-221. https://doi.org/10.1016/j.joa.2014.03.002.
- https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-8/How-to-recognise-and-manage-idiopathic-ventricular-tachycardia
- Callans D. J., Menz V., Schwartzman D. et al. Repetitive monomorphic tachycardia from left ventricular outflow tract: electrocardiographic patterns consistent with a left ventricular site of origin. J Am Col Cardiol, 1997. 29: 1023-7.
- Kamakura S., Shimizu W., Matsuo K. et al. Localization of optimal ablation site of idiopathic ventricular tachycardia from right and left ventricular outflow tract by body surface ECG. Circulation, 1998. 98: 1525.
- Hachiya H., Aonuma K., Yamauchi Y. et al. Electrocardiographic characteristic of left ventricular outflow tract tachycardia. Pacing Clin Electrophysiol, 2000. 23: 1930-4.
- Anderson RD, Kumar S, Parameswaran R, Wong G, Voskoboinik A, Sugumar H, Watts T, Sparks PB, Morton JB, McLellan A, Kistler PM, Kalman J, Lee G. Differentiating Right- and Left-Sided Outflow Tract Ventricular Arrhythmias: Classical ECG Signatures and Prediction Algorithms. Circ Arrhythm Electrophysiol. 2019 Jun;12(6):e007392. doi: 10.1161/CIRCEP.119.007392. Epub 2019 Jun 4. PMID: 31159581.
- Idiopathic Outflow Tract Ventricular Arrhythmia Ablation | AER Journal
- https://emcrit.org/emcrit/idiopathic-ventricular-tachycardia/
Published by

Assoc. Prof. Michal Pazderník, MD, Ph.D. FESC
Introduction
- Outflow tract ventricular tachycardias (OTVT) are the most common cause of idiopathic ventricular tachycardias followed by fascicular tachycardias
- Structural heart disease must be ruled out as OTVT tachycardias can manifest in patients with underlying heart disease such as myocardial infarction, arrhythmogenic cardiomyopathy or sarcoidosis
- In the absence of structural heart disease the prognosis is good
- Management of OTVT differs in RVOT and LVOT tachycardias
- The region of outflow tracts is anatomically complex and many structures can give rise to arrhythmias and precise determination of the origin may be possible only during electrophysiological study
Classification
- two types of OTVT can be distinguished:
- Paroxysmal OTVT is typically triggered by exercise or stress
- Repetitive monomorphic OTVT usually occurs at rest and presents with runs of nonsustained VTs interrupted by sinus beats
Right Ventricular Outflow Tract VT/PVC
Introduction
- RVOT is the most common origin of idiopathic VT, it represents approximately 70% of VTs in patients with structurally normal hearts and 10% of all VTs
- RVOT VT typically presents in patients 20-50 years old and affects more frequently women
- RVOT VT can also occur in patients with arrhythmogenic cardiomyopathy as the right ventricle is the most common localisation (ARVC arrhythmias do not terminate with adenosine)
- Clinical presentation can vary and it can be asymptomatic or present with palpitations or syncope. RVOT VT presents with syncope more often than LVOT VT
ECG characteristics
- Localising RVOT VT may be difficult due to the proximity of several structures acting as potential origin of outflow tract VTs (RVOT, LVOT, cusps of aortic valve, great cardiac veins, epicardial myocardium, aortomitral continuity and rarely pulmonary artery)
- Apart from typical features of a VT, the following ECG features are used to localise RVOT VT/PVCs:
- LBBB morphology
- Inferior axis
- Anterior sites in the RVOT show a dominant Q-wave or a qR complex in lead I and a QS complex in aVL. Pacing at the posterior sites produces a dominant R-wave in lead I, QS or R-wave in aVL and an early precordial transition (R/S = 1 by V3)
- Precordial transition in V3 or later and shorter R wave duration in V1 and V2 (distinguishes RVOT origin from LVOT)
- If multiple morphologies are present, scar related VT as in arrhythmogenic cardiomyopathy should be suspected
Management
- Outflow tract VT can usually be terminated by either vagal manoeuvres, adenosine or verapamil
- In symptomatic patients with RVOT VT or PVCs, catheter ablation can be highly effective and is a recommended treatment (targeting the earliest high-frequency Purkinje potential during VT)
- Patients with moderate symptoms can be treated with oral verapamil (120 mg/day to 480 mg/day)
ECG 1
- runs of non sustained VT from RVOT with interposed sinus beats
- LBBB morphology
- inferior axis (positive QRS complex in II, III and aVF)
- precordial transition in V4

ECG 2
- triplets of PVCs from RVOT
- LBBB morphology
- inferior axis
ECG 3 RVOT ventricular tachycardia (LBBB + inferior axis)
Left ventricular outflow tract VT
Introduction
- LVOT VTs account for about 10-15% of idiopathic VTs
- LVOT origin can be divided into more precise localisation including the aorto-mitral continuity (AMC), the anterior site around the mitral annulus (MA), the aortic sinus cusps (ASC), and the epicardium although these localisations are sometimes considered separately
- All of these sites of origin exhibit similar morphology due to their close anatomical proximity
- There are algorithms that can be used to precisely localise the origin of LVOT VT/PVC and it can be used in the decision to perform a catheter ablation as not all of the mentioned localisations can be successfully ablated.
ECG characteristics
- LVOT VT is suggested by LBBB morphology with inferior axis with small R-waves in V1 and early precordial transition (R/S = 1 by V2 or V3) or RBBB morphology with inferior axis and presence of S-wave in V6 (4).
- inferior axis (positive deflections in leads II, III and aVF)
- Aortic sinus cusp origin is sometimes difficult to differentiate from RVOT VT because both are so close to each other. Coronary cusp origin has to be thought when we fail an ablation in the RVOT, ECG shows a LBBB inferior axis morphology with taller monophasic R-waves in inferior leads and an early precordial R-wave transition by V2-V3.
Management
- if stable, utilize vagal maneuvers, adenosine, and/or verapamil
- chronic therapy involves beta blockers, non-dihydropyridines, class IC agents (sodium channel blockers)
- Curative catheter ablation should be considered, however, success rate of catheter ablation is lower than in the case RVOT VT/PVC and can have major complications and should therefore be performed only in highly experienced centres
ECG 1 Trigeminy of PVCs from commissure of right and left aortic cusps (curative ablation done)

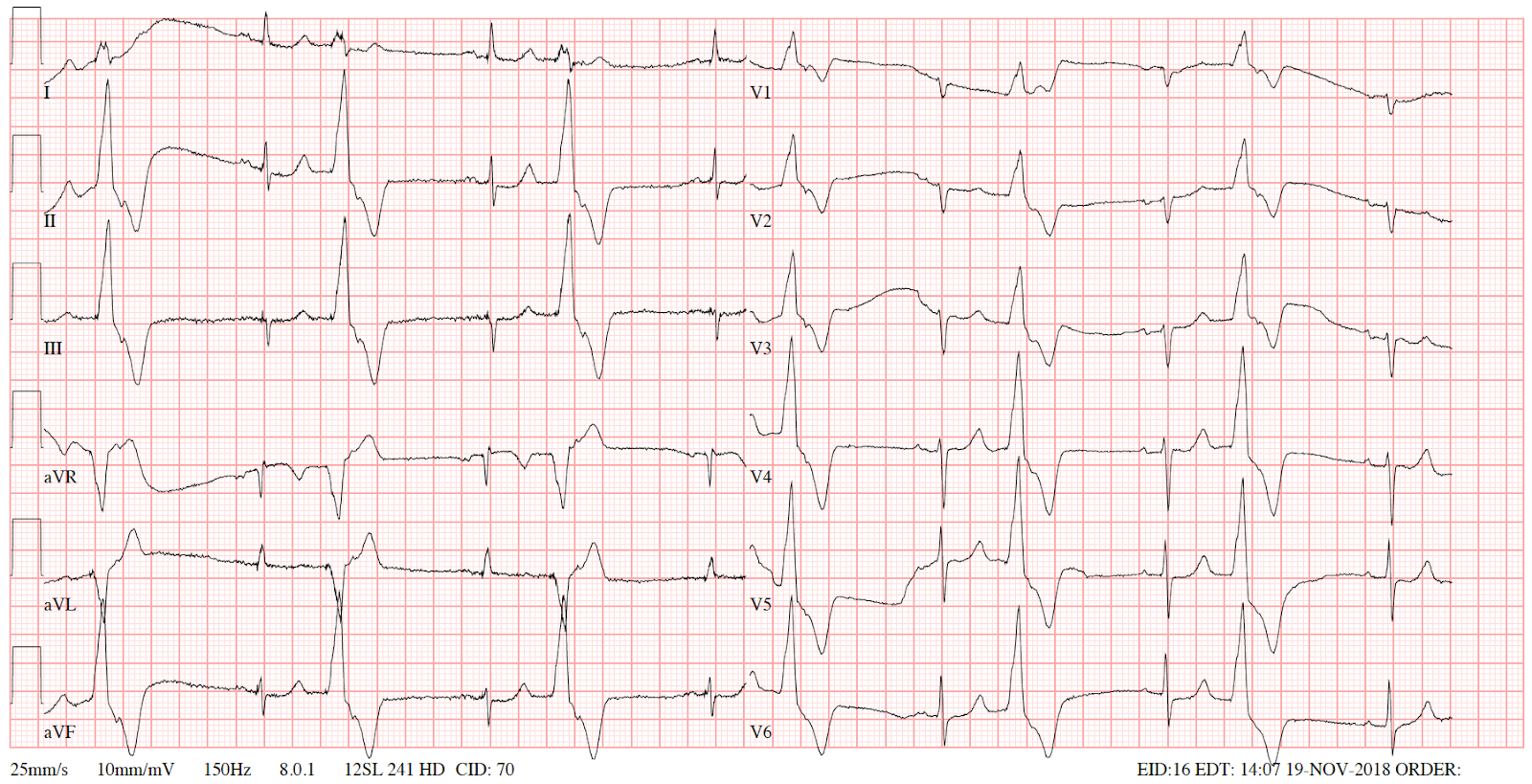
ECG 2 Bigeminy originating from LVOT (curative ablation done)
- bigeminy with PVCs of RBBB morphology in V1
- inferior axis (positive deflection in leads II, III and aVF)
References
- Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 11th ed, Zipes DP, Libby P, Bonow RO, et al, W.B. Saunders Company, Philadelphia 2018.
- Silvia G Priori, Carina Blomström-Lundqvist, Andrea Mazzanti et al. ESC Scientific Document Group, 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), European Heart Journal, Volume 36, Issue 41, 1 November 2015, Pages 2793–2867, https://doi.org/10.1093/eurheartj/ehv316
- Right Ventricular Outflow Tract (RVOT) Tachycardia • LITFL • ECG Library
- Kumagai, Koji. 2014. “Idiopathic Ventricular Arrhythmias Arising From The Left Ventricular Outflow Tract: Tips And Tricks”. Journal Of Arrhythmia 30 (4): 211-221. https://doi.org/10.1016/j.joa.2014.03.002.
- https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-8/How-to-recognise-and-manage-idiopathic-ventricular-tachycardia
- Callans D. J., Menz V., Schwartzman D. et al. Repetitive monomorphic tachycardia from left ventricular outflow tract: electrocardiographic patterns consistent with a left ventricular site of origin. J Am Col Cardiol, 1997. 29: 1023-7.
- Kamakura S., Shimizu W., Matsuo K. et al. Localization of optimal ablation site of idiopathic ventricular tachycardia from right and left ventricular outflow tract by body surface ECG. Circulation, 1998. 98: 1525.
- Hachiya H., Aonuma K., Yamauchi Y. et al. Electrocardiographic characteristic of left ventricular outflow tract tachycardia. Pacing Clin Electrophysiol, 2000. 23: 1930-4.
- Anderson RD, Kumar S, Parameswaran R, Wong G, Voskoboinik A, Sugumar H, Watts T, Sparks PB, Morton JB, McLellan A, Kistler PM, Kalman J, Lee G. Differentiating Right- and Left-Sided Outflow Tract Ventricular Arrhythmias: Classical ECG Signatures and Prediction Algorithms. Circ Arrhythm Electrophysiol. 2019 Jun;12(6):e007392. doi: 10.1161/CIRCEP.119.007392. Epub 2019 Jun 4. PMID: 31159581.
- Idiopathic Outflow Tract Ventricular Arrhythmia Ablation | AER Journal
- https://emcrit.org/emcrit/idiopathic-ventricular-tachycardia/
Published by

Assoc. Prof. Michal Pazderník, MD, Ph.D. FESC





